The shadows of trauma linger long after the immediate danger has passed, and for many men, the battle with Post-Traumatic Stress Disorder (PTSD) is a silent storm raging within. Shaped not only by the individual’s neurobiology but also by a complex weave of sociocultural threads, PTSD in men is a multifaceted ailment that demands a nuanced understanding. By delving into the neurobiological underpinnings, we unravel the synaptic tapestry of PTSD, examining how male brains are specifically altered by traumatic experiences. Complementing this scientific approach, we confront the compelling societal forces at play—stereotypical notions of masculinity that often impede men’s journey to recovery. Furthermore, we navigate together through the diverse landscape of evidence-based therapies and alternative treatments, charting a course towards resilience and post-traumatic growth. This exploration seeks not just to enlighten but to empower—offering a beacon of hope for those seeking to overcome the latent echoes of past traumas.
Neurobiological Underpinnings of PTSD in Men
Title: Unveiling the Manifestations of PTSD in the Male Brain
Understanding the complexities of the human brain remains one of the great frontiers in scientific research. Among these complexities is the impalpable nature of psychological conditions, one of which is Post-Traumatic Stress Disorder (PTSD). PTSD is a mental health disorder that can materialize after experiencing or witnessing a life-threatening event. Its manifestations within the brain, particularly in males, are of significant interest due to observed differences in PTSD prevalence and responses when compared to females.
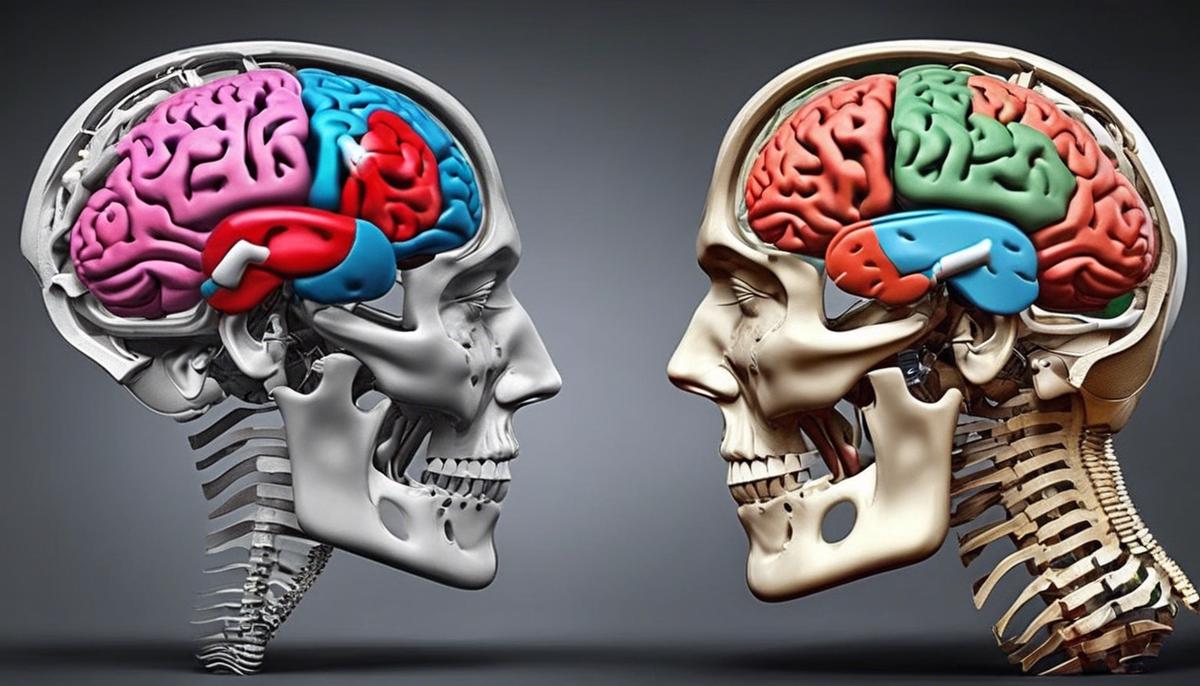
In males, PTSD is frequently linked with exposure to combat, serious accidents, or acts of violence. These traumatic encounters can leave a tangible imprint on the brain. Neuroimaging studies have identified alterations in several brain regions linked with PTSD. Among these, the amygdala, a region associated with processing emotions such as fear and aggression, often exhibits heightened activity in individuals with PTSD. This may contribute to the on-edge feeling many males describe, known as hypervigilance, and the pronounced startle response common to the disorder.
Conversely, the prefrontal cortex, which is involved in judgment and self-regulation, tends to show diminished activity in cases of PTSD. Its role includes reigning in emotional responses orchestrated by the amygdala. The deactivation or reduced functionality in this area might explain the difficulty with impulse control and decision-making that some males with PTSD experience. Furthermore, this disrupted balance between the amygdala and prefrontal cortex can lead to difficulty in extinguishing fear responses, making traumatic memories particularly intrusive and debilitating.
The hippocampus, another significant region, is responsible for the consolidation of memories. Research suggests that males with PTSD may have a smaller hippocampal volume, which could affect the ability to properly store memories and differentiate between past and present experiences. This can manifest as a tendency to relive the traumatic event as if it were occurring in the present, a symptom known as a flashback.
It is also essential to note the role of neurotransmitters and hormones in PTSD. Elevated levels of the stress hormone cortisol have been widely discussed, yet findings in males have been inconclusive due to variability in response to stress. However, some studies point to a nuanced interaction between cortisol and the hypothalamic-pituitary-adrenal (HPA) axis in males, which could influence one’s vulnerability to stress-related disorders like PTSD.
Furthermore, socialization and gender roles may influence how males with PTSD express and cope with their symptoms. While research continues to unearth the biological underpinnings of PTSD, social constructs cannot be disregarded in understanding the full spectrum of the disorder’s manifestation.
In summary, PTSD’s manifestation in the male brain involves a complex interplay of heightened emotional responses, impaired regulatory functions, and possibly, altered memory processing. The study of these neural correlates is crucial not only for developing gender-responsive treatments but also for unraveling the intricately woven tapestry that is the human mind in the aftermath of trauma. Researchers dedicated to the study of PTSD are making strides in identifying effective interventions, driven by the seminal goal to alleviate suffering and enhance the quality of life for those affected by this condition.
Sociocultural Factors Influencing PTSD in Men
The interplay between sociocultural elements and the exacerbation of Post-Traumatic Stress Disorder (PTSD) in men is a topic of considerable importance. Sociocultural factors are the characteristic elements of a society or culture that influence the thoughts, behaviors, and emotions of its members. As it pertains to PTSD in men, these factors significantly shape the way the disorder is experienced, expressed, and addressed.
Stigmatization and Societal Expectations: Within many cultures, there is a persisting stigma surrounding mental health, particularly so with men, who are often expected to adhere to traditional notions of stoicism and strength. The pressure to conform to these societal expectations can lead them to suppress emotions related to traumatic events, potentially exacerbating symptoms of PTSD by delaying or avoiding seeking treatment.
Masculine Norms and Emotional Expression: The cultural constructs of masculinity frequently discourage the open expression of vulnerability or distress. Men may feel compelled to uphold their perceived role as unflappable providers and protectors, marginalizing their emotional needs. This can result in a deeper entrenchment of PTSD symptoms as men struggle to process traumatic experiences within the confines of accepted masculine behavior.
Barriers to Seeking Help: Societal perceptions can also influence men’s willingness to seek help for PTSD. There is a pervasive belief that acknowledging the need for mental health support undermines male resiliency. This can lead to men sidelining their need for professional help, which worsens the prognosis for those with PTSD.
Veteran Status and Military Culture: Specific to military personnel and veterans—who have higher incidences of PTSD—the culture of the armed forces, emphasizing toughness and endurance, can compound PTSD symptoms. Adherence to this military ethos can deter servicemen from acknowledging PTSD symptoms and seeking necessary care.
Workplace Dynamics: In work environments where mental health issues are not openly discussed or supported, male employees with PTSD might feel isolated or discriminated against. This can create an additional layer of stress and make it more challenging for individuals to manage their condition effectively.
Intersectional Stressors: It is crucial to recognize that men do not experience PTSD in isolation from other identity markers such as race, socioeconomic status, and sexuality. Intersectionality can exacerbate PTSD when combined with other forms of systemic discrimination or marginalization, adding to the complex interplay of factors affecting mental wellness.
Sociocultural Perspectives on Treatment: Differences in cultural background can affect the perception and efficacy of PTSD treatment modalities. Men from varying cultures may have different approaches to treatment, impacting the effectiveness of standardized methods. Recognition of this diversity is essential in creating culturally sensitive therapeutic options.
In conclusion, sociocultural factors play a significant role in exacerbating PTSD among men. These influences can delay recognition, impede the pursuit of help, and cultivate an environment in which men’s mental health is minimized. Understanding these factors is critical in developing intervention strategies that are attuned to the specific needs of men with PTSD, thereby facilitating a more inclusive approach to mental health care. With a comprehensive understanding of these sociocultural determinants, researchers and clinicians can work towards creating more supportive networks and effective treatments for men struggling with PTSD, ultimately contributing to the global endeavor of mental health optimization.

Evidence-Based Therapeutic Interventions
Efficient Therapeutic Modalities for Male PTSD Sufferers
Emerging therapies for males with Post-Traumatic Stress Disorder (PTSD) have shown promise in addressing the distinct ways the disorder manifests and is experienced by this population. Paramount among treatment options is the use of evidence-based psychotherapies, such as Cognitive Behavioral Therapy (CBT) and its trauma-focused adaptation, Cognitive Processing Therapy (CPT). These treatments emphasize the identification and restructuring of maladaptive thought patterns associated with traumatic events, aligning them closer to reality and aiding in the reduction of debilitating symptoms.
Another key treatment modality is Prolonged Exposure (PE) therapy. PE encourages individuals to gradually and repeatedly face memories and stimuli associated with their trauma, thereby learning to decrease their fear response in a controlled, therapeutic setting. Over time, this exposure helps to mitigate the overwhelming anxiety linked to traumatic reminders and facilitates the extinction of fear reactions, which, as previously discussed, is a particular challenge for males with PTSD.
Eye Movement Desensitization and Reprocessing (EMDR) also plays a significant role in current therapeutic strategies. By focusing on processing distressing memories while simultaneously engaging in guided eye movements or other forms of bilateral stimulation, EMDR has been observed to facilitate the reintegration of these memories, reducing the intensity of psychological distress associated with the traumatic events.
In addition, pharmacotherapy can be an adjunct to psychotherapy, with selective serotonin reuptake inhibitors (SSRIs) such as sertraline and paroxetine frequently prescribed for PTSD treatment due to their effectiveness in managing symptoms such as anxiety and depression, which commonly co-occur with PTSD.
Group therapy, which ensures a shared space for discussing trauma and its fallout, has relevance, particularly considering societal pressures on males to conform to emotional stoicism. In this collective setting, individuals can gain peer support, understand they are not alone in their experiences, and learn from the coping strategies of others. This can be especially important in breaking down barriers to seeking help and challenging stigma.
Veteran-specific treatments address unique needs, integrating the understanding of military culture into therapy. They provide veteran cohorts with an environment that acknowledges shared experiences, potentially enhancing engagement and responsiveness to treatment options such as CBT and PE.
Incorporating mindfulness-based stress reduction techniques, which promote present-moment awareness and nonjudgmental acceptance, has shown potential in helping individuals manage the hyperarousal symptoms associated with PTSD. Mindfulness can aid in distress tolerance and emotional regulation, thereby providing a foundation of inner calm that can counteract the heightened state of vigilance commonly experienced.
The collaborative care model, involving a coordinated approach between mental health providers, primary care clinicians, and patient navigators, assists in creating an integrated system to optimize the patient’s health outcomes. It aims to alleviate barriers to accessing care and enhances consistent treatment adherence, which is essential in effectively addressing PTSD’s complex symptomatology.
Conclusively, optimal therapeutic outcomes are contingent on patient-centered approaches that consider individual patient needs, treatment preferences, and cultural factors. Multidisciplinary frameworks allow for comprehensive intervention strategies facilitating healing and recovery, tailored to accommodate the intricate dynamics of PTSD in males. With ongoing research efforts, the evolution of gender-responsive treatments continues to advance, representing a pathway towards optimal mental health and improved quality of life for male individuals living with PTSD.

Holistic and Alternative Treatment Modalities
Holistic and alternative treatments offer a complementary approach to traditional PTSD interventions for men. These treatments aim to consider the whole person—body, mind, and spirit—in the healing process. Importantly, such methods can serve as critical adjuncts to standard therapies, particularly beneficial for individuals who may find conventional treatments inadequate or unsuitable due to personal preferences, cultural beliefs, or when traditional therapies have not yielded full symptom remission.
Mindfulness and meditation practices have garnered considerable attention for their role in mitigating PTSD symptoms. Mindfulness involves a nonjudgmental, focused awareness of the present moment, which can help individuals with PTSD gain perspective on their thoughts and feelings. Mindfulness meditation can reduce the arousal associated with the sympathetic nervous system, which is often elevated in PTSD sufferers. By promoting relaxation and inner peace, mindfulness can mitigate the intrusive thoughts and hypervigilance characteristic of PTSD.
Yoga, often viewed as a physical exercise, encompasses physical postures, breath control, and meditation. Yoga’s value lies in its synergy of mind and body, offering a biopsychosocial-spiritual framework that aligns with holistic health paradigms. It provides a methodology for self-regulation, allowing PTSD sufferers to regain control of their physiological and psychological states, enhancing both flexibility and resilience.
Acupuncture, a key component of Traditional Chinese Medicine, has shown potential in regulating dysfunctional patterns in the body. With its personalized treatment protocols, acupuncture targets specific pathways, potentially adjusting imbalances in the endocrine and immune systems, which can be disrupted in PTSD.
Additionally, dietary modification and nutritional supplements can address potential biochemical contributors to PTSD symptoms. Ensuring sufficient levels of nutrients such as omega-3 fatty acids, zinc, magnesium, and B vitamins, which are essential for neurological and adrenal function, may substantially support treatment outcomes.
Peer support and community-based programs offer a unique benefit by fostering social connections. By partaking in a community, individuals with PTSD realize they are not alone, and they can share experiences and coping strategies within a supportive environment.
It is paramount to acknowledge that while holistic and alternative treatments can be remarkably beneficial, they are not a panacea. Scientific inquiry into their efficacy is ongoing, and their utilization should be tailored to each individual, ideally integrated into a comprehensive treatment plan helmed by qualified healthcare providers. The confluence of these various modalities may indeed catalyze improvement in the well-being of men with PTSD, complementing established medical interventions and promoting holistic healing.

The Path to Resilience and Post-Traumatic Growth
In the prevailing discussion of resilience and post-traumatic growth among men contending with PTSD, various avenues beyond conventional medical interventions merit scholarly attention. Delving into the fabric of psychological resilience, the constellation of factors that enable some individuals to thrive in the aftermath of trauma rather than merely survive is of essential consideration.
Social Support Networks prove pivotal in the cultivation of resilience. The presence of robust, empathetic relationships offers not just a buffer against the isolating currents of PTSD but also a reinforcement of adaptive coping strategies. Sustained emotional connections with family, friends, or support groups provide an external source of validation and understanding that can mitigate the interior tumult wrought by traumatic experiences.
Cognitive and Emotional Regulation is another cornerstone for fostering resilience. Techniques that help men articulate and process their emotions without the societal mantle of stoicism interfering are particularly efficacious. Cognitive-behavioral strategies, which involve the restructuring of negative thought patterns and fostering a growth-minded outlook, aid in transforming adversity into a catalyst for personal development.
Development of Coping Strategies and Skills is integral. Men who are equipped with an armory of coping mechanisms, both proactive and reactive, exhibit enhanced resilience. Skills such as problem-solving, assertiveness training, and stress reduction techniques empower men to confront the challenges posed by PTSD, thereby fostering a sense of agency and control.
Physical Health and Exercise have emerged as salient factors in mitigating the effects of PTSD and endorsing resilience. Regular physical activity serves as a natural antidepressant, alleviating symptoms of anxiety and depression often accompanying PTSD. It also engenders a sense of accomplishment and improves overall well-being, which can contribute to a more positive outlook on life and its stressors.
Purpose and Meaning in Life often come under duress in the wake of trauma. Yet, men who are able to ascribe meaning to their experiences, or who engage in activities that offer a sense of purpose, display higher levels of post-traumatic growth. When trauma is interpreted within a broader existential framework, it often yields a deeper appreciation for life, enhances personal relationships, and leads to a reevaluation of previously held values.
Finally, the Accessibility of Resources, both psychological and practical, such as accessible mental health services, employment assistance, and educational opportunities, plays a vital role in cultivating resilience. The amelioration of external stressors through such resources permits a more concentrated focus on recovery and growth.
Engagement with one’s traumatic experience through these lenses can often precipitate post-traumatic growth, a phenomenon wherein individuals emerge from their struggle with trauma not diminished but expanded, having developed new-found strengths, deeper relational capacities, and a more intricate understanding of their own identity.
Without a doubt, the landscape of trauma recovery and resilience is a composite one, calling for the integration of traditional and innovative approaches alike, always with a keen sensitivity to the individual at the center of the healing process. The scientific community’s continued exploration of these dynamic mechanisms holds promise in tailoring future interventions to catalyze not only the restitution of function but also the blossoming of the human spirit in the aftermath of trauma.

As we venture through the complex terrains of healing and recovery, the narrative of PTSD in men is one that transcends clinical discussion—it is a deeply human saga of struggle, strength, and eventual triumph. The road to resilience is paved with knowledge, understanding, and the unwavering pursuit of personal growth. Embracing holistic and therapeutic approaches, men grappling with PTSD can not only reclaim their lives but can also experience profound personal transformation, emerging stronger and more self-aware. Through the support of loved ones, healthcare professionals, and their own indomitable spirits, they rewrite their stories, transforming them from tales of adversity to epics of survival and growth. The odyssey of overcoming PTSD thus becomes a testament to the indelible spirit of mankind and a powerful reminder that even in the aftermath of our darkest hours, there lies the potential for a dawn filled with purpose and hope.
